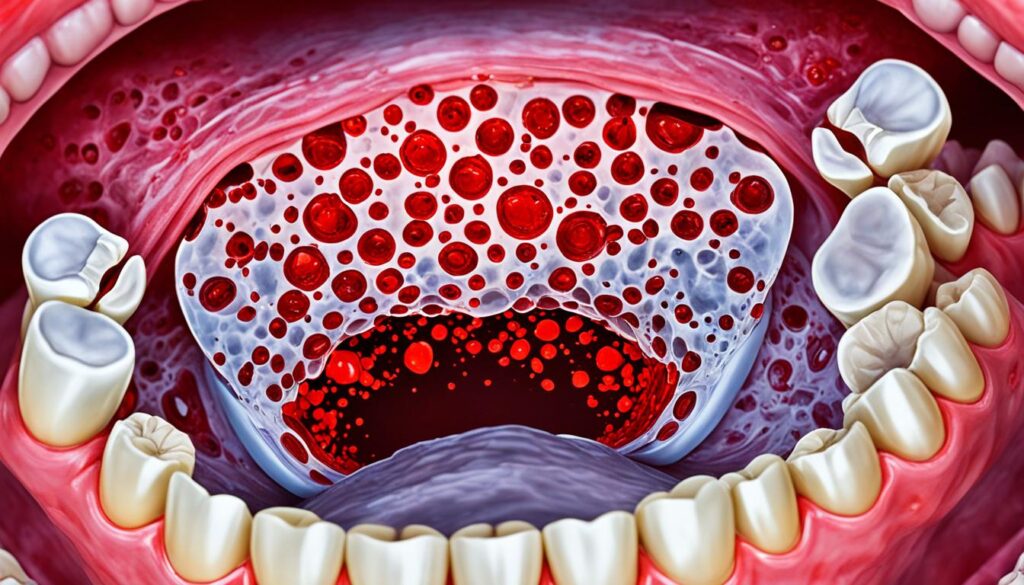
Have you seen red spots on the roof of your mouth and wondered why? These spots can look scary but they’re often harmless. They usually disappear without any treatment. In some cases, they might signal a health problem you need to take care of.
Many things can trigger these red spots. Eating or drinking hot, spicy, or acidic items is a common factor. These foods and drinks irritate the mouth’s soft tissues. This irritation can cause red spots to form.
Infections like strep throat are another reason for these spots. A bacteria known as Streptococcus can cause petechiae, tiny red spots. These are joined by other signs like a fever, swollen tonsils, and trouble swallowing.
Oral thrush is a fungal infection that can turn the roof of your mouth red. Nearly everyone has the fungus that causes thrush in the mouth. Under certain conditions, it can grow unchecked, leading to red spots and discomfort.
Sometimes, viral infections, including herpes simplex virus (HSV), are behind these spots. HSV is very common. It affects almost half of people aged 14 to 49. This virus can lead to cold sores, which also appear as red spots in the mouth.
Most often, you don’t need to worry about red spots in your mouth. They usually disappear without help. But if they stay or you’re worried about your health, see a doctor or dentist. They can check and make sure everything is okay.
Key Takeaways:
- Red spots on the roof of the mouth can be caused by irritation from certain foods, infections like strep throat, oral thrush, or viral infections like herpes simplex virus (HSV).
- While most red spots are harmless and will go away on their own, it’s important to seek medical attention if they persist or if there are concerns about an underlying health condition.
- Maintaining good oral hygiene by brushing teeth twice daily and visiting the dentist regularly is essential for improving overall oral health and preventing various oral health conditions.
Strep Throat
Strep throat is a throat infection caused by Streptococcus bacteria. It’s common in children aged 5 to 15. About 30% of kids with a sore throat in winter and early spring have it.
One sign of strep throat is red spots called petechiae on the mouth’s roof. These spots happen because of the bacteria’s inflammation.
Other symptoms include a fever over 101°F, throat pain, and swollen neck nodes. The tonsils may get red and swollen too.
Doctors check for strep throat with throat cultures for better accuracy than rapid tests. This confirms if Streptococcus bacteria are the cause.
Antibiotics are the usual treatment if you have strep throat. Medicines like penicillin or amoxicillin clear the infection. It’s vital to finish the antibiotics, even if you feel better.
Not treating strep throat can lead to serious issues. This includes abscesses, swollen lymph nodes, and even kidney disease. So, it’s important to see a doctor and follow their advice.
Sources:
- Johns Hopkins Medicine. (n.d.). Strep Throat. Johns Hopkins Medicine. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/strep-throat
- Centers for Disease Control and Prevention. (2021, February 25). Group A Strep Infection. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/groupastrep/diseases-public/strep-throat.html
Sudden Injury or Trauma
Sometimes, red spots or sores on the roof of the mouth come from sudden injuries. For instance, a cut or burn from eating or drinking hot things. These can be painful and make you feel uncomfortable.
Other times, the cause might be something that doesn’t fit right, like dentures. Even broken teeth or being sensitive to some toothpaste can lead to mouth injuries.
Most small mouth injuries get better in a few weeks by themselves. To speed up healing, it’s best not to irritate the area more.
If these red spots or sores last longer, it’s wise to visit the dentist. They can figure out why it’s happening and help with the right treatment.
Caring for your teeth well and acting fast on any problems is key to staying healthy. This includes keeping your mouth clean and checking any problems early.
Oral Thrush (Oral Candidiasis)
Oral thrush is a yeast infection from the fungus Candida. It’s common across all ages but babies and older adults might catch it more. If your immunity is low, either from health conditions or certain drugs, you’re more at risk.
If you have poorly controlled diabetes, you’re also at risk. This is because sugar in your spit helps candida grow. Wearing dentures, especially upper ones, and having a dry mouth can make you more likely to get oral thrush.
Rarely big trouble for the healthy, oral thrush can be bad news for those who are already sick. It might even spread throughout the body. Untreated, it can hurt when swallowing, especially for those not so healthy.
Signs and Symptoms
Thrush shows up suddenly. You might see creamy white spots appearing anywhere in your mouth. These spots come with redness and might be sore. You could lose your taste or feel like your mouth is full of cotton.
If it gets really bad, swallowing becomes painful or hard. Some might even get a fever. Thrush can become more than a mouth problem for those with weak immune systems, reaching the lungs or skin.
Treatment and Prevention
Treating oral thrush means fixing what’s making your immunity weak. Healthcare pros will likely give you antifungal meds. These can be creams, lozenges, or even liquids to get rid of the fungus.
To keep from getting oral thrush again, there are things you should do. Rinse after using corticosteroid inhalers. Keep your mouth clean by brushing and flossing well. See your dentist often and watch your sugar if you have diabetes.
It’s also important to treat vaginal yeast infections quickly. These can sometimes lead to oral thrush. Keep your mouth from getting too dry. Drink enough water, quit tobacco, limit alcohol, manage stress, and use moisturizers for your mouth.
Following these tips and treating health issues early can cut your risk of candida infections. This way, you’ll protect your mouth and overall health.
Mouth Ulcers
Mouth ulcers, or aphthous ulcers, are common sores in the mouth. They make eating and drinking hard. Dehydration, poor hygiene, smoking, and certain foods can cause them. They can also be linked to health issues like Crohn’s disease, celiac disease, and HIV.
These sores usually last 2-4 weeks. They can be painful. Eating soft foods and avoiding certain foods can help. Avoid foods that can make the pain worse.
“Mouth ulcers can be quite painful and interfere with daily activities. It is important to take measures to alleviate discomfort and support the healing process.”
Often, mouth ulcers aren’t serious and go away on their own. But, if they last a long time or other symptoms appear, see a doctor. They can help with the pain and any needed treatments.
Prevention of Mouth Ulcers
To lower your risk of mouth ulcers, there are things you can do:
- Keep your mouth clean by brushing and using mouthwash.
- Avoid tobacco, as it can make mouth sores more likely.
- Drink enough water to keep your mouth moist.
- Eat a balanced diet that’s good for your teeth.
- Talk to your doctor about medication side effects that can cause mouth ulcers.
By taking these steps for good oral health, you could avoid the pain of mouth ulcers. Keeping your mouth clean and healthy is the best defense.
Hand, Foot, and Mouth Disease
Hand, foot, and mouth disease (HFMD) is a viral illness. It mainly affects kids under age 5 but can also strike older children and adults. The disease comes from coxsackieviruses and other viruses in the digestive system. This includes the mouth, throat, stomach, and intestines. HFMD shows itself with a fever, sore throat, drooling, and a rash.
Its symptoms usually show up within a week of being near someone with the virus. It can spread through the air, especially in the first week of illness. This is why containing it early is key.
The illness doesn’t stop at a rash. It can lead to red spots in the mouth, turning into painful blisters. These blisters can make eating or drinking hard. It could even cause dehydration or seizures in severe cases.
There’s no vaccine for HFMD yet. But, you can lower the risk by washing hands often and keeping things clean. Covering your mouth and nose when you sneeze is important, too.
Prevention is vital to curb hand, foot, and mouth disease. Regular handwashing and surface cleaning can keep this viral illness away.
Dealing with HFMD means managing its symptoms. There’s no direct treatment, but medicine can help with fever and pain. It’s important to drink a lot if you have it, to prevent dehydration.
If a child has HFMD, it’s best to keep them home until they get better. Most kids recover in about a week. But if things don’t improve, calling the doctor is wise.
When talking to a doctor about HFMD, ask about how long it’s contagious. Also, ask about the chance of scarring and when it’s safe to go back to work if you have kids.
Herpes Simplex Virus (HSV)
The herpes simplex virus (HSV) causes cold sores or fever blisters. They appear around the lips or inside the mouth, even on the roof. Starting as white or red spots, they can be painful.
HSV spreads easily, especially when it’s active. It can be passed through touch or by sharing personal items. Being careful can stop its spread.
Cold sores usually go away within two weeks. During this time, take care of your mouth. Avoid doing things that could make it worse.
Cold sores can come back more often in the first year. But they usually become less severe and less frequent. This happens as the body learns to fight the virus.
If you see red spots on your mouth’s roof and feel pain or itching, see a doctor. They can diagnose and suggest the right treatment.
Preventing Herpes Transmission
- Avoid close physical contact with individuals who have active cold sores.
- Do not share personal items such as lip balm or razors.
- Practice good hand hygiene by washing hands regularly.
Genital herpes (HSV-2) can spread even if infection signs aren’t visible. Those with it should take care to prevent others from getting it, notes the CDC. This is especially important during outbreaks.
Treatment Options
For oral herpes, treatments include over-the-counter cold sore medicines. There are also antiviral creams and pills like acyclovir. For pain, nonsteroidal anti-inflammatory drugs (NSAIDs) can help.
In severe cases, like widespread HSV or encephalitis, someone might need to stay in a hospital. Special herpes cases in infants (neonatal herpes) also need quick medical attention.
Seeing a doctor regularly is key. They’ll offer the best advice and treatments for managing cold sores.
Canker Sores
Canker sores, known as mouth ulcers, are small sores in the mouth. They begin as red bumps with a white or yellow center and a red border. Though they can hurt, they are not usually a big worry. Most canker sores heal on their own in 1-2 weeks.
Their exact cause is not fully clear, but several things might lead to them. These can be things like viral infections, stress, and even mouth injuries. Some people are more likely to get them. This includes those with weak immune systems, vitamin deficiencies, or bowel issues like Crohn’s.
There are medicines you can buy without a prescription that can help. Topical anesthetics and mouth rinses with antimicrobial properties can ease pain and speed up healing. Always follow the instructions and see a doctor if the sores don’t get better or if you have other worrying symptoms.
Avoiding things that make the sores worse can also help. Stay away from acidic or spicy foods that can make the pain worse. And remember, keeping your teeth clean with a soft brush is important. This helps stop more irritation.
Usually, canker sores go away on their own. But if they keep coming back or if they are severe, it’s best to see a doctor. They can give you the right advice.
Erythroplakia
Erythroplakia is a red patch or spot found often in the mouth. Its exact cause is unknown, but it shows up more in people who use tobacco or drink a lot. Typically, it affects men between 60 and 70 years old.
It looks like smooth, velvety patches with clear edges. These patches might make your mouth burn and taste like metal. Seeing a doctor is crucial because these signs could mean oral cancer.
Half of these cases could turn into squamous cell carcinoma, a serious oral cancer type. Getting help early is very important.

Using tobacco greatly ups your chance of getting this condition. Cigarettes and chewing tobacco expose your mouth to dangerous chemicals. This leads to erythroplakia.
Big drinking is also a risk for oral lesions like erythroplakia. Drinking and smoking together make the risk even higher.
Removing the abnormal tissue can stop cancer from growing. Antifungal meds treat non-cancerous types if they’re caused by infection. Good oral hygiene and care may stop erythroplakia.
Remember, most erythroplakia lesions can’t just be scraped off. This is why it’s key to get professional medical help.
Color Changes in the Mouth
Changes in the color of your mouth might show something is wrong. Sometimes, the change is not too obvious. By visiting a dentist or doctor, you can make sure everything is okay. There are many reasons this might happen, such as:
- Anemia: A type of anemia can lead to mouth sores and color changes in the mouth. People with anemia might feel tired often and have pale skin.
- Infections: Infections like hand, foot, and mouth disease can make the mouth have red blisters. Viruses, like the one causing cold sores, can also change the mouth’s color.
- Oral Conditions: Issues like oral leukoplakia, which shows as white patches, can cause color changes. Conditions such as lichen planus may lead to various color changes too.
- Mouth Cancer: White or red areas that persist in the mouth could be signs of cancer. It’s especially worrying if they are with soreness, numbness, or trouble eating or swallowing.
A wide range of things can cause the mouth’s color to change. For instance, smoking or not taking care of your teeth may do it. If you see strange color changes that don’t go away, talk to a healthcare provider. This is the best way to figure out what’s going on and how to treat it.
Keeping your mouth healthy means seeing the dentist often. Also, you must brush and floss daily. Doing this helps keep your mouth looking and feeling good, without any unusual color changes.
Maintaining Oral Hygiene
Keeping your mouth clean is key for good health and avoiding dental issues. Here are tips to keep your smile bright:
- Brush your teeth twice daily: Brush your teeth with fluoride toothpaste twice daily to remove bacteria and food. This prevents cavities and gum problems.
- Use mouthwash or rinse regularly: Add mouthwash to your daily routine to fight bacteria and make your breath fresh. Choose a mouthwash with healthy ingredients.
- Avoid tobacco products: Smoking and chewing tobacco can harm your teeth and gums, cause bad breath, and increase cancer risk. Quitting is vital for your oral health.
- Manage medication side effects: Some medicines can lead to dry mouth, which can harm your teeth. Drink plenty of water and ask your doctor how to lessen this effect.
- Visit the dentist regularly: Seeing the dentist often helps stop problems before they start. Aim for check-ups and cleanings twice a year.
Prevention is the Key
“Prevention is better than cure.”
Good oral care can stop issues like cavities and gum disease. These healthy habits, along with a balanced diet and being active, boost your overall health and keep your teeth strong.
Your mouth’s health is crucial to your well-being. Make oral hygiene a top concern by using these steps. This way, you’ll keep smiling and avoid many oral troubles.
Conclusion
Red spots on the roof of the mouth can be caused by many things. These include canker sores, strep throat, and injuries. Hand, Foot, and Mouth Disease, oral herpes, and oral thrush are also common causes. If red spots don’t go away or cause other issues, you should see a doctor or dentist.
Preventing these spots is important. You can do this by keeping your mouth clean. Brush your teeth often and see your dentist. Stay away from hot, spicy, and acidic foods. Also, don’t use tobacco. This makes you less likely to get red spots.
If you already have red spots, the right treatment is key. For some, this may mean taking antibiotics or antifungal medication. With the right care, these spots can be cleared up. Don’t ignore any spot that doesn’t disappear. Always get it checked by a professional. Regular dental check-ups are also crucial. This helps catch any problems early. And remember, taking care of your mouth is a big part of staying healthy.